Thrombosis is a serious condition where one or more blood clots form in your blood vessels or heart. When this happens, the clot can block blood flow where it formed, or it can break loose and travel elsewhere in your body. If a moving clot gets stuck in a critical area, it can cause life-threatening conditions like stroke and heart attack.
Thrombosis is the formation of a blood clot (thrombus) inside one of your blood vessels or a chamber of your heart. Clots can block blood flow in your blood vessels or break free and travel elsewhere in your body. If a clot gets stuck in a critical location like your lungs or brain, it can disrupt blood flow to that organ and result in a life-threatening emergency. Symptoms vary based on the clot’s location and can include chest pain, trouble breathing and skin changes.
Some people face a higher risk of thrombosis due to medical conditions or other factors. Learning your risk can help you prevent thrombosis, and learning the symptoms can help you recognize problems if they occur. Thrombosis is a serious condition, and it can become more dangerous as time passes. It can quickly turn into a medical emergency. The sooner you seek care for thrombosis, the better your chances of a good outcome. If you or someone with you has symptoms of thrombosis, seek emergency medical care immediately.
Thrombosis can lead to many different complications depending on where the blood clot forms or travels to:
The two main types of thrombosis are:
Thrombosis is dangerous in either location (artery or vein) because it can:
Thrombosis is extremely common and is the underlying cause of 1 in 4 deaths worldwide. That’s because thrombosis can lead to dangerous conditions like a heart attack, stroke or pulmonary embolism.
Thrombosis is more common among people with certain medical conditions, including:
Thrombosis symptoms depend on the size of the clot, its location (where it forms or gets stuck) and the complications it causes. Blockages are more likely to occur in areas with very small blood vessels, especially your lungs, brain and farther down in your legs and arms. Listed below are common symptoms for each location:
Thrombosis happens when something damages the inner lining of your blood vessel (endothelium) or slows blood flow. In either case, cells in your blood start to stick together when they shouldn’t.
Normally, many cells in your blood coexist in harmony and come together when needed for a certain job. For example, if you have a wound, platelets and proteins join together at the site of injury to serve as a plug. This multistage process (hemostasis) forms a necessary clot that stops you from losing too much blood. The clot dissolves when your wound heals. It’s like an emergency meeting at work when everyone huddles at one desk. When the problem’s solved, everyone leaves and goes their separate ways.
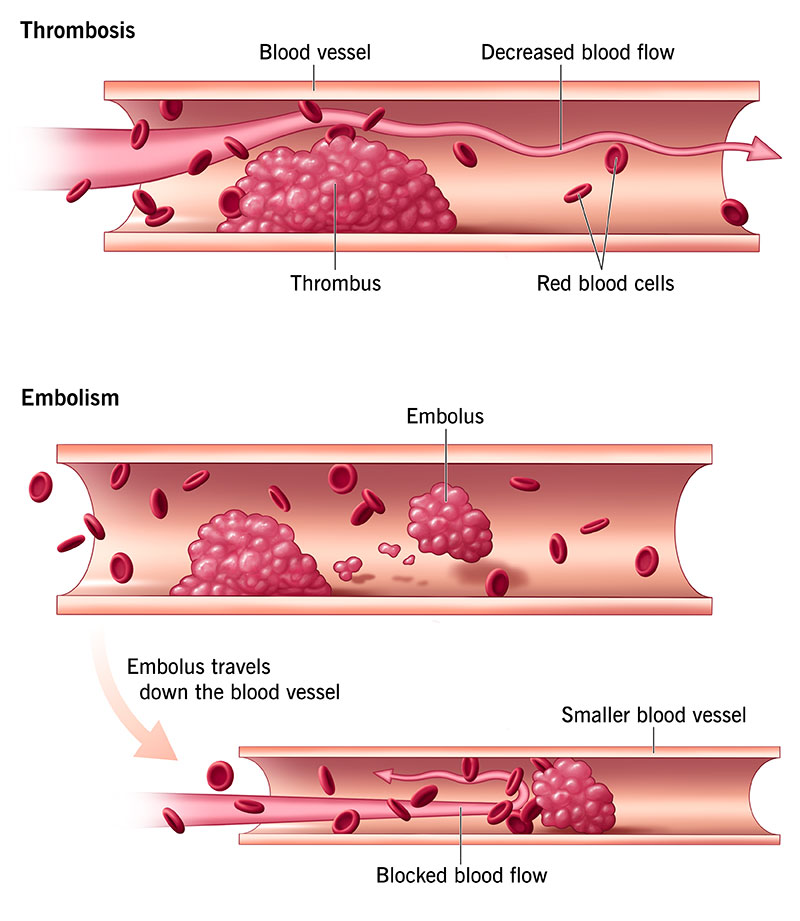
But various medical conditions, medications and other factors can cause components of your blood to cluster together when they don’t need to or fail to dissolve when they should. As a result, a blood clot (thrombus) may form from clumps of blood clotting components and potentially get bigger. It may also break away and travel through your bloodstream until it gets stuck in a smaller blood vessel (embolus).
Both of these situations can lead to dangerous — or even life-threatening — complications. That’s why it’s important to learn what may put you at risk.
Anything that interferes with your blood’s ability to flow freely or clot normally can raise your risk for thrombosis. This includes many conditions, medications and lifestyle factors.
Early diagnosis and treatment can restore your blood flow and lower your chance of complications. If a complication (like a heart attack or stroke) leads to your diagnosis, your provider will treat that condition and do whatever possible to restore function to affected organs and tissues.
It depends on the underlying cause, the treatments and how quickly you seek medical attention. Thrombosis can be short-lived with prompt treatment. However, the conditions that cause it may be chronic or lifelong. For example, blood clotting disorders that you’re born with may put you at risk for thrombosis throughout life. Your provider can help you manage underlying conditions to lower your risk.
Your outlook or prognosis depends on many factors, including:
A clot that stays in place is a problem, but it’s usually less dangerous than a clot traveling in your bloodstream. The outlook for thrombosis can worsen when a free-floating clot ends up in a critical organ like your heart, brain or lungs.
Your provider can tell you more about your prognosis based on your individual situation.
If you’ve had thrombosis in the past or are at risk, it’s crucial to:
Call 911 or your local emergency number if you have symptoms of thrombosis. Don’t delay. Thrombosis can very easily become a dangerous, life-threatening condition. The more minutes that pass, the greater the risk of complications.